Prior authorization is broken. Simply put, 95% of physicians stated that prior authorization is somewhat, or significantly, increasing their burnout [AMA]. Payers and providers are drowning in administrative burdens, leading to member dissatisfaction and delays in patient care.
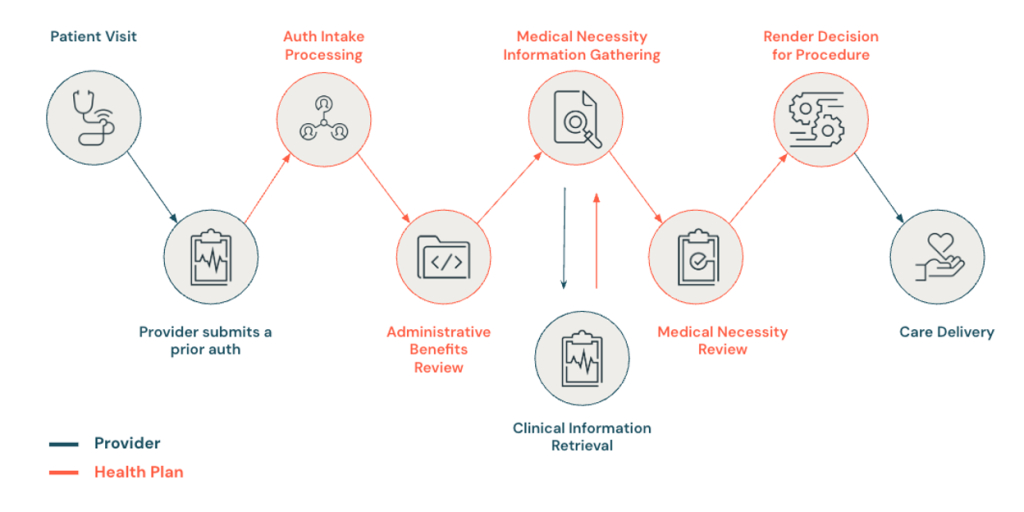
Prior authorization is a key activity that providers engage in to obtain approvals from health plans before a medical service or medication can be prescribed to a member or patient. The workflow is so burdensome because it’s a multi-step process that requires coordination across multiple stakeholders.
What if we can automate the prior authorization workflow by leveraging the potential of all of the data end-to-end? At a recent Databricks interoperability workshop, Redox joined industry leaders to discuss how data intelligence and interoperability can modernize prior authorization workflows.
Data is a major bottleneck to prior authorization
Healthcare is mired in outdated, disparate legacy standards. The complexities of managing and harmonizing platforms and standards make most data siloed and ineffective. Furthermore, cohesive data governance is also a major challenge and risk.
Despite so many advancements in healthcare, prior authorization workflows are tedious and largely manual. For providers, staff must work with multiple portals, dealing in high volumes of paper documents and faxes. More than 1 in 3 (35%) of physicians have staff who work exclusively on PA, spending 12+ hours per week on submissions and appeals alone [AMA].
For payers, prior authorization is an important tool to ensure that members are getting affordable, evidence-based care [AHIP]. But claims teams manually read, interpret, and validate both portal and paper inputs, often resulting in slow and disjointed decisions. Data extraction from unstructured formats also plays a major role in slowing down processing.
These inefficiencies and lack of access to the right data at the right time lead to delays, denied claims, and administrative overhead, ultimately impacting patient outcomes.
Redox’s approach to prior authorization (PA) modernization
Our strategic cloud partnerships connect our customers to ecosystems like the Databricks Data Intelligence Platform. Through Redox’s real-time data exchange, payers and providers can leverage data intelligence in Databricks to drive actionable decisions with AI-supported solutions. Our deep industry expertise and accelerated implementation timelines make it faster for customers to see tangible business impact to their PA workflows.
According to CAQH, by adopting fully electronic transactions across healthcare administrative processes like PA, the industry could save more than $18 billion annually. Leave outdated paper-and-fax processes in the past and level up with data-driven automation.
With joint PA solutions powered by Redox and Databricks, payers can:
- Reduce effort for compliance with CMS-0057-F mandates
- Aggregate real-time clinical data to support faster PA decisions; automation can reduce data entry and eligibility verification burden
- Automate gold carding for providers
- Reduce integration effort for multiple providers that request PAs
Providers can:
- Reduce manual work and eliminate faxing
- Save an average of 11 minutes per transaction
- Integrate seamlessly with AI solutions for superior decision-making
- Support PA within the existing clinical workflow (SMART on FHIR, CDS Hooks, and more)
What’s next
By partnering with Redox and Databricks, payers and providers can transform their outdated prior auth processes into streamlined, data-driven workflows. We’ll also announce more exciting interoperability advancements for our partnership, including augmenting and expanding the reach of our network through TEFCATM participation.
Watch the full healthcare interoperability workshop, and learn more about how Redox + Databricks are delivering better healthcare outcomes.